Protein in Parkinson’s provokes the immune system
Bits of a protein that builds up in Parkinson’s disease trigger the immune system, causing it to tag them as foreign invaders.
In a blood test, immune cells called T cells became activated when exposed to the protein in about 40 percent of Parkinson’s patients in a new study. This autoimmune response may contribute to the progression of the disease, the researchers report online June 21 in Nature.
Neurodegenerative disorders like Parkinson’s “have not really been thought of as autoimmune disorders,” says coauthor David Sulzer, a neuroscientist at Columbia University and the New York State Psychiatric Institute in New York City. “The data strongly indicate that we better look at autoimmune responses as at least one of the links in the chain of developing Parkinson’s.”
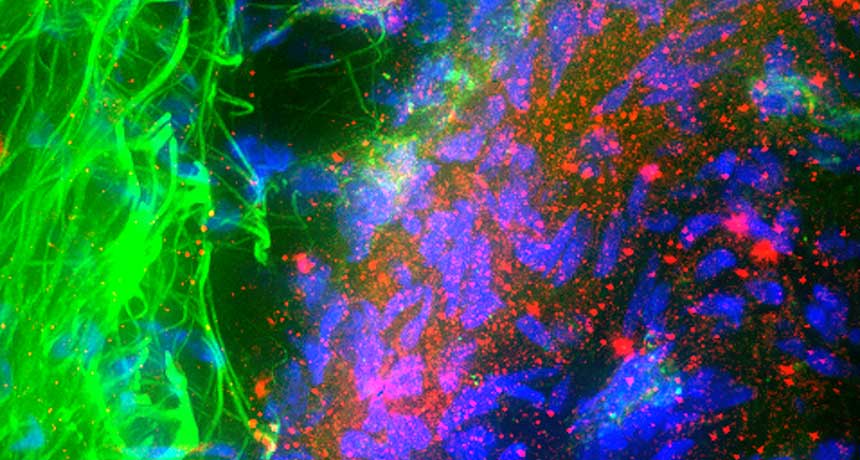
Patients with Parkinson’s experience tremors and slowed movement, among other symptoms. Scientists don’t know exactly what causes Parkinson’s, but during the disease, many nerve cells located in a region of the brain called the substantia nigra die. These neurons release dopamine, a chemical messenger that is sent to other parts of the brain to coordinate movement. Little blobs known as Lewy bodies, primarily made of a protein called alpha-synuclein, also build up in these neurons.
One of the immune system’s jobs is to distinguish between the body’s own components and foreign substances, such as bacteria and viruses. Certain types of immune cells capture proteins and present them to T cells, which figure out, “Is it self? Or is it nonself? Does it come from bacteria, a virus or some kind of invader?” Sulzer says. In autoimmune disorders, the immune system makes an error in judgment.
Sulzer and colleagues had previously discovered that the substantia nigra neurons that release dopamine can present proteins to T cells, if given a signal from the immune system. If the body cannot degrade alpha-synuclein properly, bits of these proteins that build up in the nerve cells could end up being presented to T cells, which might see them “as not being self, even if it comes from you,” Sulzer says. In the new study, the researchers tested for an immune response to two different, small stretches of the alpha-synuclein protein using blood samples from 67 people with Parkinson’s and 36 healthy people.
Indeed, the two pieces of alpha-synuclein were essentially recognized as foreign by T cells in Parkinson’s patients, Sulzer says. He speculates that the autoimmune response contributes to the progression of the disease, rather than the start, as it’s triggered by the inability to properly break down alpha-synuclein.
“As with any good study, there are more questions than answers,” says neuroscientist Andrew West of the University of Alabama at Birmingham. Assuming the work can be replicated in other Parkinson’s patients, “the question becomes: When do these changes in immune cell activation become apparent? Early in the disease, or later?” he says.