New twist on a flu vaccine revs up the body’s army of virus killers
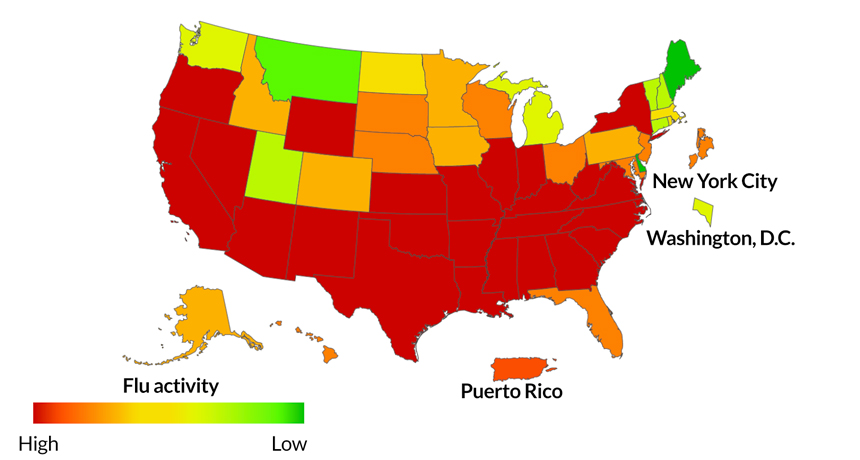
Sometimes an old fight needs a new hero. With the United States in the midst of a tough flu season — and with evidence from Australia that the current flu shot is only 10 percent effective against the strains responsible for most illnesses — a different approach to flu vaccine development may do the trick.
Vaccines traditionally protect against illness by stimulating antibodies to block viruses. In the case of influenza viruses, this strategy can fall short: Influenza antibodies are specific to one strain, which may not be among the strains causing illness during an outbreak. Instead, researchers developed a flu vaccine that ensures influenza viruses can’t escape the body’s first line of defense, a powerful antiviral system that enlists a cadre of immune proteins and cells.
“Because the virus is more visible to the host immune system,” says Ren Sun, a virologist at UCLA, “it stimulates a very strong immune response.”
Mice vaccinated with the newly designed influenza virus, called hyper-interferon-sensitive (HIS) virus, survived exposure to lethal doses of several different influenza A strains. But the majority of those exposed but not vaccinated with HIS died, researchers report in the Jan. 19 Science.
“This was a tour-de-force study,” says John Teijaro, a viral immunologist at the Scripps Research Institute in La Jolla, Calif., who coauthored a perspective that accompanied the article. The researchers exploited vulnerabilities in the genetic material of influenza viruses to create a weakened virus that can still kick-start the immune system. The approach may be useful to devise vaccines for other human pathogenic viruses, he says.
The new vaccine targets the body’s type I interferon system. When a virus invades a cell, one of the body’s first signals that it’s under attack comes from type I interferon proteins, which then rev up the production of hundreds of proteins that fight the virus. Immune cells called T cells are also activated, in order to kill infected cells. While T cells cannot prevent infection, they reduce the virus’ ability to grow and spread in the body.
Viruses, including influenza, have proteins that inhibit the type I interferon proteins. Sun and his colleagues looked for influenza strains that were sensitive to the antiviral machinery and identified mutations behind the susceptibility. Sun’s team then combined eight of these mutations into one HIS virus, the basis for an attenuated viral vaccine, one that has a weakened but live version of the virus.
Sun and colleagues vaccinated 40 mice with the HIS virus vaccine. After 28 days, they exposed those mice and another 40 not vaccinated with HIS to lethal doses of one of four different influenza A strains — three from the H1N1 subtype and one from the H3N2 subtype (H3N2 viruses are causing much of the misery this flu season). All of the vaccinated mice survived, while most of the other mice died, depending on which flu strain caused their infection.
T cells are thought to be able to provide protection across different strains, says Teijaro, because the bits of influenza virus the T cells recognize do not mutate as much as the influenza surface proteins, the target of antibodies. But “the breadth of protection against numerous influenza strains was not investigated here,” and will be important work for the future, he says.
Teijaro adds that the ideal approach may be to combine the HIS virus vaccine with a strategy to generate broadly neutralizing antibodies — those that can bind many different influenza strains — to create a universal flu vaccine (SN: 10/28/17, p. 18).